How Artificial Intelligence Can Help Your Prostate Gland
Artificial Intelligence is making your life better and easier in so many ways it’s hard to keep track. Think of conveniences like a fast internet search, your safest and fastest GPS routes, cybersecurity, etc. You may even have benefited from improved medical practice efficiency in terms of your health records and appointment setting. Did you ever stop to consider what AI can contribute to a man’s health, specifically the wellness of his prostate gland?
The walnut-size prostate is essential for a man’s fertility as well a sexual pleasure. It manufactures the fluid that carries sperm out of the body during orgasm. Because of its role in reproduction, Nature has protectively tucked it away; most men rarely if ever think about it until it poses a problem. If that problem happens to be prostate cancer, a disease that affects 1 out of every 8 men in his lifetime, suddenly the gland demands his attention. Like any cancer, it is potentially life-threatening. However, if found early, treatment success rates approach 100% at five years.
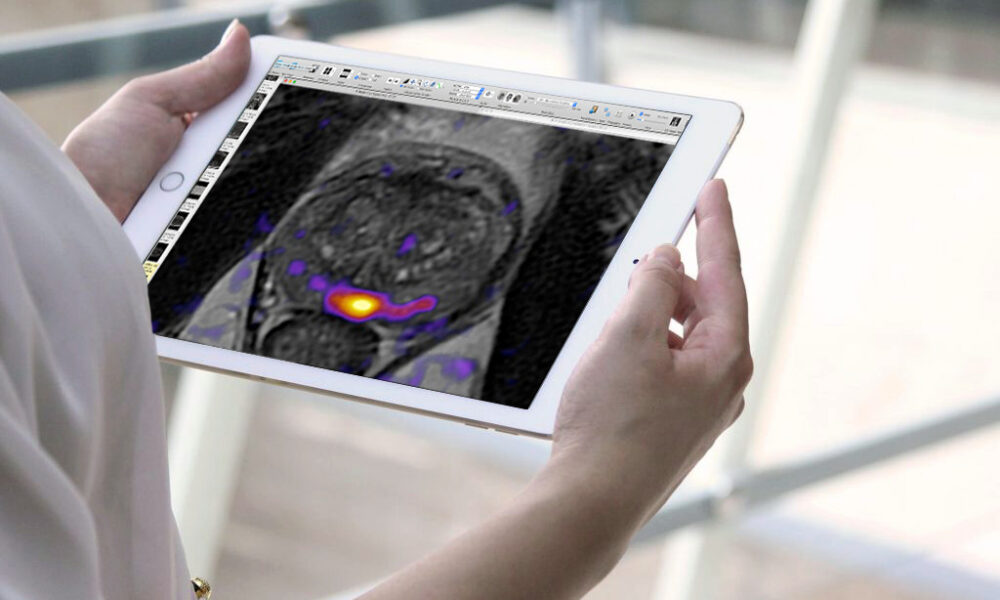
Besides the importance of early detection, a swift and accurate diagnosis is the key to making the best treatment decision. There are two essential tools for diagnosing prostate cancer: a special scan called multiparametric MRI (mpMRI) that gives a 3-dimensional detailed portrait of a patient’s prostate, and a needle biopsy targeted to what the mpMRI shows. Without these, a definitive diagnosis can’t be made, yet the treatment must match the extent and aggressiveness of the cancer cells.
Two obstacles to achieving the best match are
1) Inefficient workflow. Radiologists who read the MRI scans, and pathologists who analyze microscopic tissue samples from a needle biopsy are often overwhelmed with their workload, and the time it takes to interpret the data in front of them.
2) Errors in human judgment. Studies have shown that experience matters, and less seasoned radiologists and pathologists have greater error rates.
While a patient’s MRI is waiting to be read and reported on in writing, and the biopsy slides are in transit to a busy laboratory, it’s not yet known if the patient’s cancer is indolent (a term meaning relatively slow growing) or aggressive. Aggressive cells are not lazy, they are growing. Until all the information is back, a doctor can’t rightly advise his patient on a treatment strategy—and the patient grows more anxious.
Here’s where AI comes to the rescue. Hundreds of AI programs are in international development. They incorporate Machine Learning or Deep Learning to read and interpret MRI scans or digital biopsy slide images for the red flags that signal cancer. When properly trained and clinically tested, such programs proceed with lightning speed to identify prostate tumors and assign an aggression level to them. In fact, many are already approved and commercially available. Clinical tests have repeatedly demonstrated that AI performs with diagnostic accuracy at the same level as experienced radiologists and pathologists, while handling hundreds of cases with breathtaking rapidity.
Here are few examples of products and what they are capable of:
1) 43 published studies of various Machine Learning or Deep Learning programs that can extract quantitative data from MRI scan features found products that could correctly predict the Gleason Grade Group assigned to biopsy samples. (The Gleason Grade Group is a 5-tier system to rate the aggression level of the cancer cells).
2) Prior to prostate cancer surgery (prostatectomy) a Machine Learning model based on MRI scans plus other patient clinical factors calculated the likelihood that the patient would have erectile dysfunction after surgery. This helps doctors and patients discuss future quality of life and alternative treatments before making a final decision.
3) Machine Learning trained on specially labeled biopsy slides of prostate tissue can evaluate image features that correlate with Gleason Grade Group, helping to formulate a treatment strategy. There are also models that use such features to predict treatment outcomes, for example, would a patient facing radiation treatment be more likely to benefit by also taking a course of hormones?
These are just a few of the ways in which AI has the potential to help doctors and patients generate the best treatment choice. Ultimately, the best match has the most promise of success with the least probability of treatment side effects. Thanks to AI, not only are men’s lives saved, but patients also enjoy the quality of life they hope for after treatment.
NOTE: This content is solely for purposes of information and does not substitute for diagnostic or medical advice. Talk to your doctor if you are experiencing pelvic pain, or have any other health concerns or questions of a personal medical nature.